

Head and Neck Cancers predominantly affect adults and are not the most common cancers in Singapore and Southeast Asia. In fact, the Singapore Cancer Registry of 2018 shows that only thyroid cancer made the top ten most common cancers in women (placed 8th, accounting for 3.9% of all female cancer cases in Singapore or 300 cases a year). In men, no head and neck cancer made the top ten by incidence but nose cancer was placed 8th by mortality (accounting for 3.3% of all cancer deaths in men or 100 deaths per year)
Head and neck cancers can cause significant morbidity as they can affect the ability to breathe, eat and talk.
The following are the common head and neck cancers that I manage:
What are the risk factors for head and neck cancers?
There are many dietary and lifestyle factors that increase one’s risk of head and neck cancers. These include:
The key aspects of optimizing outcomes in head and neck cancer are:
I trained in several central and west London hospitals and was fortunate to have mentors in head and neck cancer surgery who were world famous surgeons and excellent teachers. They were Professor Tony Cheesman at Charing Cross Hospital who sparked my interest in head and neck, and anterior skull base surgery. Professor David Howard at the Royal National Throat Nose and Ear Hospital who introduced transoral laser microsurgery to the United Kingdom, and from whom I learnt many techniques in this field. As the Senior Registrar at the Royal Marsden Hospital, I worked with Mr Peter Rhys-Evans and Mr Peter Clarke who were excellent oncological surgeons. The Royal Marsden is the oldest cancer hospital in the world and boasts some of the finest surgeons in the UK. It was here that I met the visiting Professor William B Coman of the Princess Alexandra Hospital in Brisbane, Australia. His unit treats the largest number of head and neck cancers in Australasia and I subsequently became his fellow in 2007. At the Princess Alexandra, I further developed my knowledge and skills in treating oral cavity and laryngopharyngeal cancers.
During my tenure as Consultant and Chief of the Head and Neck Cancer Service at Tan Tock Seng Hospital (TTSH), I had the opportunity to further my training in robotic surgery. I completed advance training in transoral robotic surgery (TORS) and robotic thyroidectomy at Severance Hospital in Seoul, South Korea. I also undertook basic and advanced training in ultrasound of the neck and thyroid with the American College of Surgeons in San Francisco in 2010 and Boston in 2017. I initiated the head and neck ultrasound service within the Department of ENT in TTSH. I routinely use in-office ultrasound for the comprehensive assessment and monitoring of the neck in all my head and neck cancer patients.
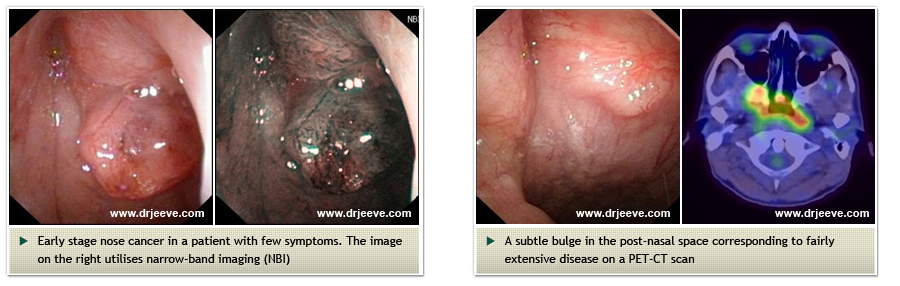
Nose cancer is common in Southeast Asia. Singapore has one of the highest incidence of nose cancer in the world. People from South China (particularly the Cantonese) have a high incidence of this tumour. A diet rich in nitrosamines (which is present in salted and preserved foods) and infection early in life by the Epstein-Barr Virus (EBV) contribute to this cancer.
One of the problems with nose cancer is that the tumour causes few symptoms in the early stages of disease. When advanced, it causes nasal congestion, nose bleeds, neck lumps, deafness and double vision. The survival outcome from this cancer is best when diagnosed and treated at an early stage. Early diagnosis is therefore important. The best method for screening for nose cancer is to perform flexible nasal endoscopy of the nose and nasopharynx. Narrow band imaging is sometime helpful in identifying early lesions and blood tests for cancers markers are useful too particularly in relatives of patients with nose cancer.
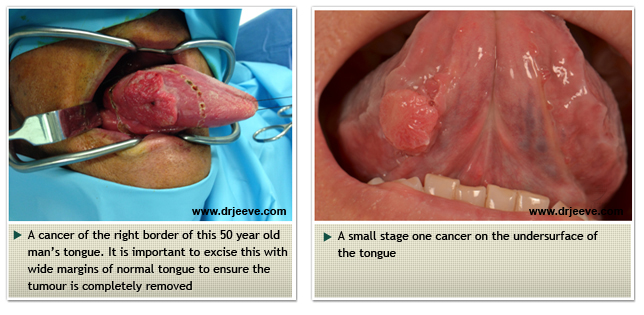
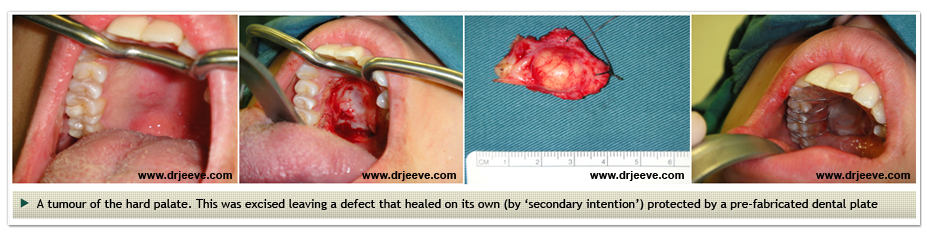
Cancers of the oral cavity include tongue cancer, cancers of the floor of mouth and gum. These cancers are often due to chronic irritation of the lining of the mouth. Hence, smoking, alcohol consumption, chewing betel nut, sharp teeth and conditions such as lichen planus and Fanconi's Anaemia may all cause oral cavity cancers.
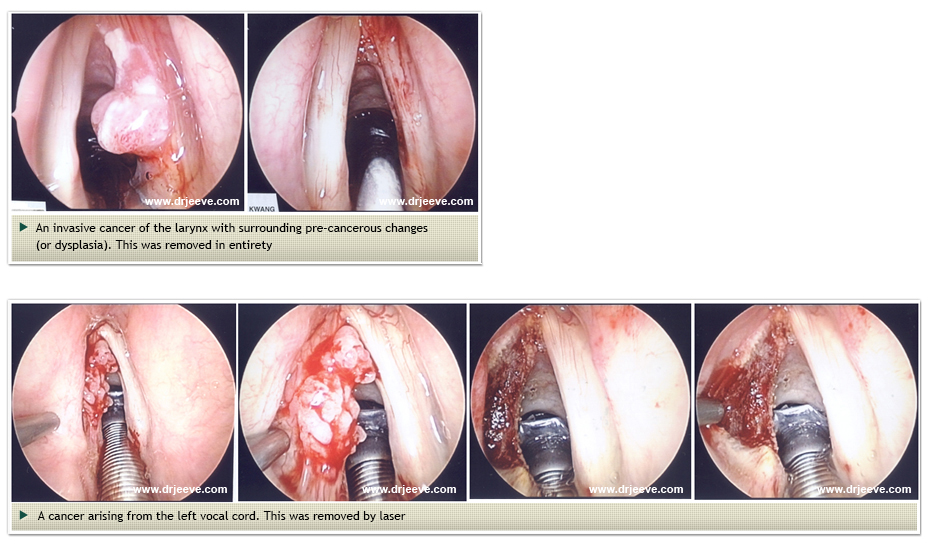
Cancer of the larynx is intimately related to smokers. Smoking one pack of cigarettes a day increases your risk of larynx cancer by seven fold. Larynx cancer fortunately presents early as it causes hoarseness. Cancers of the larynx when large may cause airway obstruction and noisy breathing (called stridor).
Early stage cancer of the larynx may be treated by surgical removal. This can be achieved effectively with the use of Carbon Dioxide (CO2) laser. The voice quality, although poor to begin with, is equivalent to that achieved with radiotherapy. For advanced stage cancers, radiotherapy with chemotherapy is often used except in extensive disease where it is necessary to remove the larynx. This is an operation called laryngectomy (see my lecture handouts)
Surgery to remove cancers of the head and neck are technically challenging. The anatomy of the head and neck is extremely complex. These are some of the common operations I undertake: